Chronic wounds: a silent epidemic requiring urgent attention
The Aalto-Helsinki 2022 is a multidisciplinary and international group consisting of 10 people from both the University of Helsinki and Aalto University.
This article is part of the innovation theme.
edited by Kenia, Reviewed by carmine, illustration by Usha. read by nelly.
We all know the discomfort of having a wound after a fall: the throbbing pain when our skin is first injured, the care we must take to keep it covered and disinfected, the itchiness while it heals. But wounds can form for reasons other than accidental injury and remain open for much longer than the typical couple of weeks, sometimes even for over three months. These are called “chronic wounds “, and chances are that you haven’t heard of them though they will likely affect you directly or indirectly in the future.
Globally, up to 2% of the population experience chronic wounds in their lifetime – that’s 160 million people. Not without reason, they are sometimes referred to as a “silent epidemic”. They are not only a burden to the patient but entire healthcare systems. In developed countries, they account for between 3 and 5.5% of healthcare expenses. Within the EU, up to 50% of hospital beds are occupied by patients with wounds, and though this refers to a mixture of acute and chronic injuries, the latter take up greater resources due to the many in- and out-patient follow-ups.
Chronic wounds are often caused by other underlying chronic diseases, and, as you can imagine, the pain and discomfort they cause are many times greater than typical wounds. In diabetes, their leading cause, excessive blood sugar (“hyperglycemia”) is linked with stiffer blood vessels, which in turn leads to slower circulation and other blood vessel dysfunctions. As a result, when extremities – especially the feet – are injured, less oxygen and immune cells can reach the wound site. As the immune system struggles to provide nutrients for healing, the open wound becomes more vulnerable to infections.
So, what can be done to manage these chronic wounds and hopefully decrease their burden on patients and health systems? This is what we, the Aalto-Helsinki iGEM team of 2022, are looking into.
iGEM is a worldwide synthetic biology competition that enables motivated student research groups to develop a solution to a pressing local or global problem. We decided to enter this competition and represent both Aalto University and the University of Helsinki, combining our diverse backgrounds across medical sciences, design and engineering to construct a novel treatment for this chronic wound epidemic.
Given that different patients rarely respond to the same treatment, we first needed to find a common trait of most chronic wounds to create a standardised, single-application solution. We knew that one of the reasons these types of injuries are unlikely to heal within normal timelines or follow common tissue re-growth stages is their infection with bacteria, which develops over time into a layer called ‘biofilm‘.
Biofilms are structural communities of one or more types of microorganisms growing on a surface. They can build up wherever there is insufficient removal of microbes, which means that you are more familiar with them than you think. They are the slimy film that develops on an overused toilet, the plaque that builds up on teeth that aren’t brushed enough, or the bacterial layer on a chronic wound, where the immune system cannot ‘clean out’ the site fast enough.
Biofilms are present in around 80% of chronic wounds and further contribute to their slowed healing. As the biofilm thickens, the accumulated bacteria become dormant. This may intuitively sound like good news, but in fact, it leads to further complications. Dormant bacteria have decreased metabolic activity, which in short, means less production and usage of the energy that sustains the daily activities of an organism. This slowed metabolism makes dormant bacteria more tolerant to antimicrobials, which usually act on these same metabolic, energy-generating pathways. This is why many chronic wound treatment methods have minimal effect and why the patient’s quality of life is dramatically reduced.
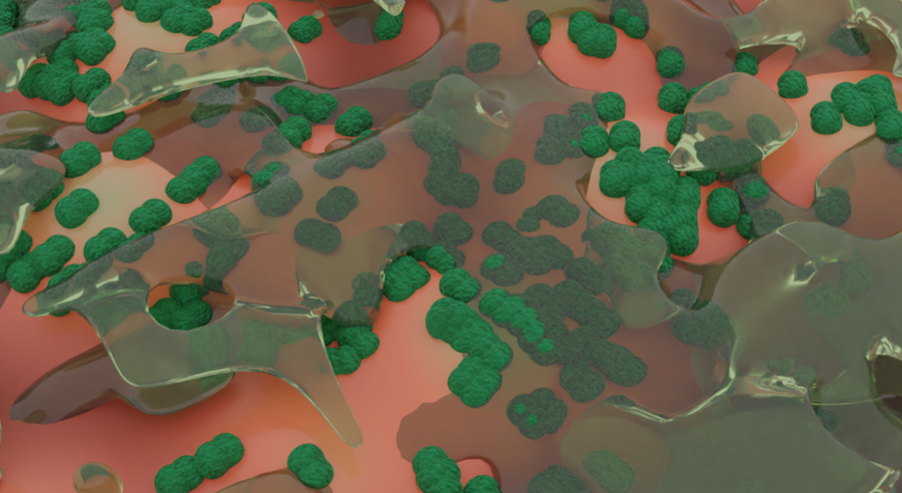
Since biofilms are present in chronic wounds of almost all causes, we decided to focus on targeting and halting their formation. Going through the academic literature, we found the specific bacterial signalling mechanisms underlying the process, giving us a more precise inhibition target for our therapy. Bacteria that first attach to the wound communicate with other bacteria nearby through a process called “quorum sensing“, encouraging them to settle on the same site. If we could block this communication channel, biofilm formation should be prevented, making chronic wounds less likely to be infected and more likely to heal.
Despite having limited time and resources as a student team, we dove into how we could make innovation into reality to impact the patient’s treatment. Discussions with clinicians from HUS Wound Centre helped us to shape our project so that it would follow a “cell to patient” research line. Through them, we better understood the distinctions between acute and chronic wounds, the extent of their public health burden, and the difficulties physicians and patients face in treating them. Introducing our project idea to people in the field, we also gained encouraging feedback: our potential solution could be helpful in a hospital setting.
As chronic wound prevalence increases due to population ageing and obesity, the problem is not anticipated to get easier in the future. In any case, we are confident that raising awareness about chronic wounds will make the public more conscious of their importance and encourage further cutting-edge research to develop a lasting treatment.
Our research journey continues, and we will be ready to present our working product, Q Block, by the end of 2022. Meanwhile, one of our goals is to reach different communities through social media. If you want to follow our journey, you are welcome to look at our Instagram, Twitter, Facebook, Linkedin, Tiktok accounts and our webpage, biweekly blog and podcast.

REFERENCES
Høiby, N., Bjarnsholt, T., Givskov, M., Molin, S., & Ciofu, O. (2010). Antibiotic resistance of bacterial biofilms. International journal of antimicrobial agents, 35(4), 322-332.
International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International. 2022.
Järbrink, K., Ni, G., Sönnergren, H., Schmidtchen, A., Pang, C., Bajpai, R., & Car, J. (2017). The humanistic and economic burden of chronic wounds: a protocol for a systematic review. Systematic reviews, 6(1), 1-7.
Malone, M., Bjarnsholt, T., McBain, A. J., James, G. A., Stoodley, P., Leaper, D., … & Wolcott, R. D. (2017). The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. Journal of wound care, 26(1), 20-25.
Mendoza, R. A., Hsieh, J., & Galiano, R. D. (2019). The impact of biofilm formation on wound healing. Wound healing-current perspectives, 10.
Nunan, R., Harding, K. G., & Martin, P. (2014). Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Disease models & mechanisms, 7(11), 1205-1213.
Posnett, J., & Franks, P. J. (2008). The burden of chronic wounds in the UK. Nursing times, 104(3), 44-45.
Rutherford, S. T. and Bassler, B.L. (2015). Bacterial Quorum Sensing: Its Role in Virulence and Possibilities for Its Control. Cold Spring Harbor Perspectives in Medicine.
Spampinato, S. F., Caruso, G. I., De Pasquale, R., Sortino, M. A., & Merlo, S. (2020). The treatment of impaired wound healing in diabetes: looking among old drugs. Pharmaceuticals, 13(4), 60.
Stokes, J. M., Lopatkin, A. J., Lobritz, M. A., & Collins, J. J. (2019). Bacterial metabolism and antibiotic efficacy. Cell metabolism, 30(2), 251-259.
Wang, Y., Armato, U., & Wu, J. (2020). Targeting tunable physical properties of materials for chronic wound care. Frontiers in Bioengineering and Biotechnology, 8, 584.